IVF Perth
In-Vitro Fertilisation (IVF)
Welcome to Fertility North, a leading IVF clinic in Perth, Western Australia. For over 20 years, we have provided IVF treatment to individuals and couples facing challenges in conceiving.

What is IVF?
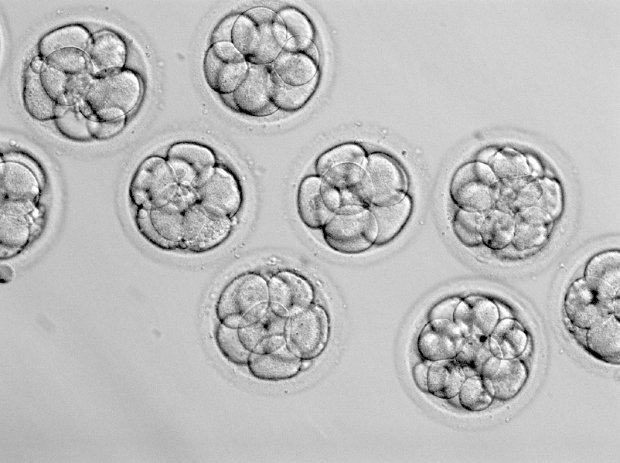
IVF, or in vitro fertilisation, is a specialised infertility treatment designed to assist with conception by bypassing the eggs journey from the ovaries to the uterus. It has been in use for over 40 years, and is the most well-known, and most successful form of fertility treatment available. The process involves combining eggs and sperm outside the body in a laboratory setting, in vitro (“in glass”). Once fertilisation occurs, the resulting embryo/s are monitored and developed (Embryo Culture) until it is ready to be transferred to the uterus, offering a chance for pregnancy.
Why you might consider IVF treatment
As IVF bypasses the need for the egg to travel from the ovaries to the uterus, IVF was originally used to treat blockages in the fallopian tubes, however, there are now many reasons to pursue IVF as your main form of fertility treatment.
Fallopian Tube Damage or Blockage
IVF provides an alternative when fallopian tubes are damaged, preventing an egg from being fertilised or an embryo from travelling to the uterus.
Severe Endometriosis
Endometriosis causes endometrial tissue, the cells that normally line the uterus, to grow outside the uterus, which can potentially affect the function of the ovaries, uterus, and fallopian tubes. Because IVF bypasses damaged fallopian tubes, it increases the chances for successful pregnancy.
Uterine Fibroids
Fibroids can alter the uterine cavity, hindering embryo implantation and growth. This can be improved using IVF as embryo implantation chances can be increased by selecting high-quality embryos for transfer.
Ovulation Disorders
Conditions like Polycystic Ovary Syndrome (PCOS), hypothalamic dysfunction, premature ovarian failure, or excessive prolactin can disrupt regular ovulation, making natural conception less likely. IVF controls the ovulation process, maximising the availability of eggs for fertilisation, making it especially useful when other treatments like ovulation induction have not been successful.
Male Factor Infertility
Those suffering with low sperm count, poor sperm motility, or abnormalities in sperm size and shape are often left with lower natural fertilisation chances. IVF, especially when combined with ICSI (Intracytoplasmic Sperm Injection), can overcome these issues.
Genetic Disorders
Couples at risk of passing on genetic disorders can opt for IVF combined with preimplantation genetic testing (PGT) to ensure healthy embryos are selected, reducing the risk of transferring a genetic disease.
Fertility Preservation
For those undergoing gonadotoxic treatment like chemotherapy or gender reassignment, which might affect fertility, IVF allows for embryo or egg freezing for future family planning.
Same-Sex Couples or Single Individuals
IVF can be part of assisted reproductive technology (ART) solutions, like using donor sperm or eggs, for those wishing to have children but are limited by biological constraints.
Age Related Infertility
As women age, egg quality and quantity are generally seen to decline, and this decline accelerates beyond the age of 35. IVF allows us to select the healthiest embryos and maximise the chances of pregnancy.
Unexplained Infertility
In some cases, there are no identifiable causes for being unable to conceive. In these cases, IVF allows couples to be proactive earlier and enhance their chances of pregnancy by controlling fertilisation and implantation processes.

Why choose Fertility North?
Our clinic has made significant contributions to the advancement of IVF treatment, evidenced by our published research in peer-reviewed scientific journals. This commitment is a result of our ongoing desire and ability to question and enhance existing methodologies and medical practices. By choosing us as your IVF treatment provider, you know you are working with a highly experienced and successful team of fertility specialists in Perth.
Meet our dedicated IVF specialists
Our team at Fertility North consists of over 40 talented and fully accredited staff members, including Fertility Specialists, Scientists, IVF Nurses, Fertility Counsellors, and support staff. Our Team is dedicated to assisting our clients on their journey to parenthood.


What will IVF cost?
At Fertility North we publish our fee structure online, without any hidden fees. We also try to minimise out of pocket expenses for our patients to make IVF treatment more affordable.
As of August 2023, your first IVF cycle will cost $8950, with an estimated out of pocket cost of $4843 through Original Medicare Safety Net (OMSN) or $2882.10 though Extended Medicare Safety Net (EMSN). Please ensure you refer to our updated fee structure for the latest in cycle fees and Medicare rebates.
The benefits of IVF
IVF has become the world’s most successful form of fertility treatment due to its ability to treat infertility in a diverse range of situations, but its benefits extend even further than just flexibility.
Effectiveness
IVF has proven itself to be a highly effective treatment for infertility in a wide range of cases, including issues with ovulation, sperm quality, fallopian tube blockages, and unexplained infertility. It can also be used in conjunction with donor eggs and donor sperm for those with specific fertility or genetic issues.
Genetic Screening
The use of Preimplantation Genetic Testing (PGT) during the embryo selection phase will identify embryos unaffected by selected genetic disorders, significantly reducing the risk of genetically inherited diseases.
Multiple Pregnancy Chances
IVF allows for the creation and replacement of embryos across multiple cycles. For example, one IVF cycle may yield 5 viable, good quality embryos allowing you up to 5 embryo transfers. This increases the likelihood of pregnancy compared to natural conception or other fertility treatments where typically only one egg is ovulated each time.
Increased Success Rates
Fertility North utilises the latest in reproductive technology, including sophisticated monitoring and laboratory techniques, which enhance the likelihood of successful fertilisation and embryo development.
FAQs
What are the risks associated with IVF
While there are many benefits of IVF, there are risks you should be aware of when considering whether IVF is right for you.
Ovarian Hyperstimulation Syndrome (OHSS)
Some women may over-respond to fertility drugs used in IVF, leading to OHSS, characterised by swollen, painful ovaries. While mild cases are common, severe OHSS is rare but serious.
Emotional and Psychological Impact
The IVF process can be emotionally challenging, involving significant physical, emotional, and financial commitments, which can lead to stress and anxiety.
At Fertility North, we do much more than “just” IVF. Alongside our world-class fertility treatments and advanced technology, we offer a comprehensive range of fertility preservation and support options for our patients.
Ectopic Pregnancy
Although rare, there’s a risk of ectopic pregnancy, where the embryo implants outside the uterus, most commonly in a fallopian tube.
Multiple Births
There’s an increased chance of twins or triplets with IVF, primarily due to the transfer of multiple embryos. This can lead to complications such as preterm birth and low birth weight. To mitigate this risk, Fertility North adheres to requirements set out in the RTAC Code of Practice in which single embryo transfer is the preferred option in many cases.
Advanced Parental Age
Research shows that advanced parental age is associated complications such as diminished ovarian reserve, elevated sperm DNA fragmentation, reduced fertilisation and pregnancy rates, pre-eclampsia, gestational diabetes, autism and chromosomal anomolies.
Should I try other fertility treatments first?
The decision to proceed with IVF depends on individual factors like age, health conditions, and previous fertility treatments. Our specialists will guide you through these considerations to make an informed choice.
How long does IVF take?
Start to Finish
A typical IVF cycle, from consultation to embryo transfer, spans about 6-8 weeks.
To Get Pregnant
The time taken to achieve a successful IVF pregnancy varies. Some may succeed in their first treatment cycle, while others may need multiple cycles. Unfortunately, IVF treatment may not be successful for all patients.
What are the alternatives to IVF?
Other treatments like IUI or OI may be suitable for some. We’ll explore all options with you to find the treatment that offers you the best chance of success.
What are the predictors of success?
Success in IVF is influenced by factors like age, lifestyle, and specific fertility issues. Your Doctor will assess your individual circumstances to provide you with a realistic outlook and optimise your chances of success.
Is IVF hard on the body?
The impact of IVF varies greatly from one person to the next. Some patients find the process is easily tolerated, while others will find it challenging from a physical and/or an emotional perspective. Our Team is here to support you however you find the treatment journey.
What happens after IVF pregnancy?
For those patients who conceive using IVF treatment, your ongoing pregnancy can be managed by your GP, midwife, public maternity hospital or private obstetrician, the choice is yours! The same can be said for your method of delivery or childbirth and beyond.
Can you choose gender with IVF?
Gender selection for family balancing or social reasons is not permitted in Australia.
Can you ask for twins with IVF?
Due to the fact that multiple pregnancies are associated with an increase in maternal and foetal risks, the goal of IVF treatment is to achieve a healthy, singleton pregnancy and this is supported by our industry’s code of practice.
Is IVF insertion painful?
The collection of egg from the ovaries by surgical means is usually associated with some level of discomfort. This is usually easily managed using over the counter pain relief, such as paracetamol. The transfer of an embryo back into the uterus is a little bit like having a cervical screening test, and while not pleasant, it is generally very well tolerated and does not require any pain relief.
Who should avoid IVF?
Unfortunately, in accordance with state and federal regulation, we are unable to offer IVF treatment to those who are infertile due to advanced parental age alone.